Like hundreds of OTs, I am one of the many licensed occupational therapists working in the United States during the COVID-19 outbreak. Outside of the rehabilitative profession, I am also a full-time parent and an active community participant. To say times are strange would be a gross understatement. What does an OT’s world look like during 2020?
Pulmonary Rehabilitation Shift: What it Means for OTs and Patients
For OTs who have worked directly with patients with COVID-19, you’ve probably noticed a weird shift in your job description: pulmonary rehabilitation specialist. In fact, this isn’t a shift at all but rather an opportunity to highlight respiratory qualifications and skills as it relates to function.
While working in intensive care, some of us have been asked to join pulmonary rehab teams in order to promote patients’ typical breathing patterns. Not only are we asked to assist with bed mobility transfers, but also to facilitate handling and positional techniques to optimize a patients’ respiration needs and to clear, sometimes lethal, gunk from their lungs.
Post-COVID-19 Intervention
Once our patients with COVID-19 have graduated from intensive care and no longer test positive for the virus, OTs have some additional interventions to offer.
Remember, this is a virus that seriously deprives the body of oxygen for lengthy periods of time. You can expect muscle weakness, fatigue, balance issues, cognitive changes, and reduced activity tolerance post-COVID-19.
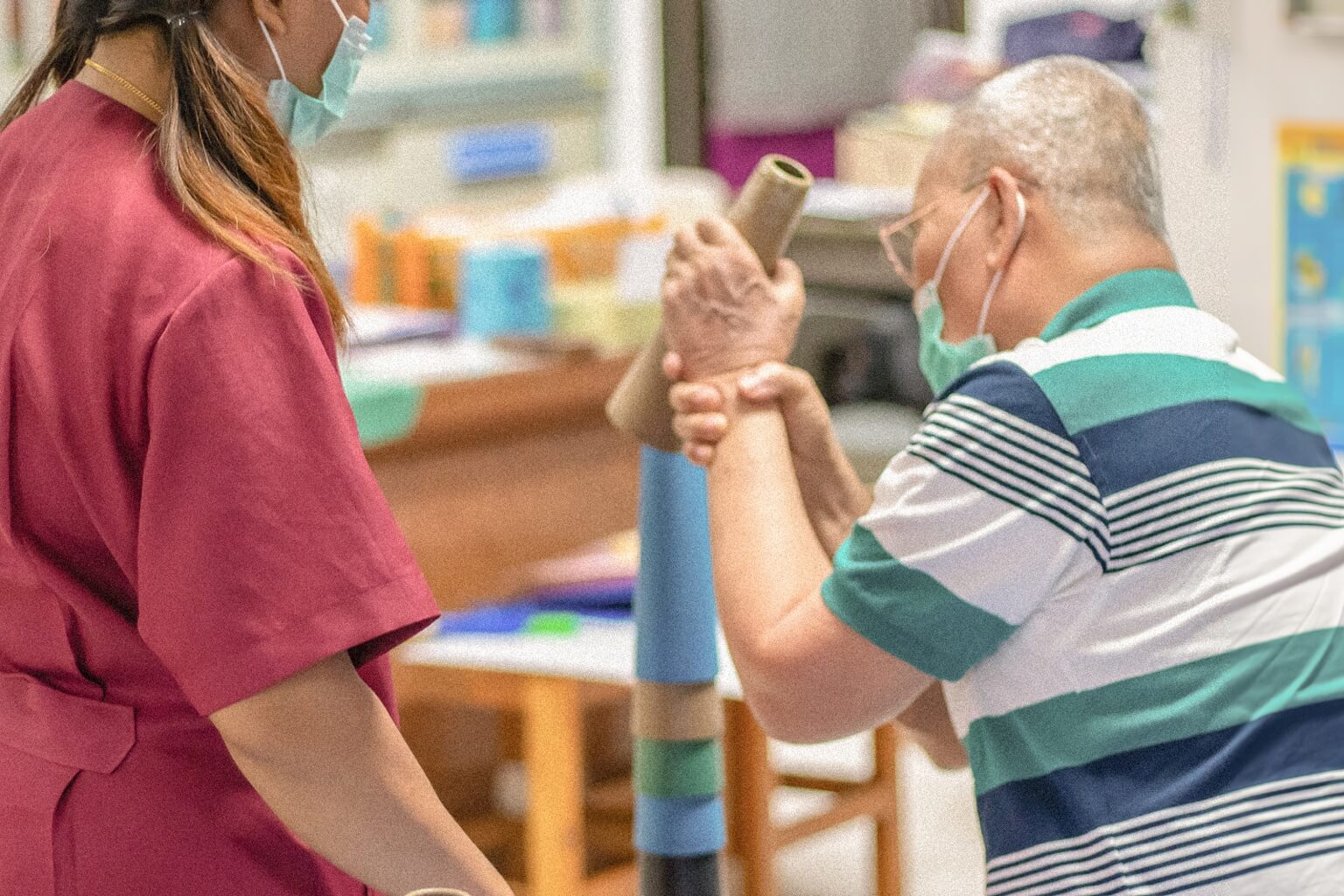
During inpatient, skilled nursing, transitional care, and/or home health rehab, OTs can provide our patients with therapeutic activities and strategies to help them get back to their normal lives.
Group Therapy Modifications
Group therapy is common for adult care settings, including skilled nursing, transitional care, and assisted living facilities. Patients benefit from each other by working together through intervention strategies specific to their needs.
Depending on where you live and work, group therapy has either been indefinitely canceled or extremely modified to meet the CDC’s social distancing requirements. Although OTs can still carry out successful group therapy and concurrent therapy sessions, their activity choices are severely limited for the sake of sanitation and disease prevention.
Billing/Insurance Process Changes with Telehealth Advancement
Telehealth is becoming an extremely important tool during this pandemic. Telehealth regulations and insurance waivers specifically for the pandemic have become permanently signed in under an executive order this year.
This order is a major stepping stone for healthcare workers in the world of virtual healthcare. Now we can ethically perform interventions and evaluations via telehealth with ethical billing and insurance practices. Many states have been passing similar legislation to accommodate for the pandemic and maintain these virtual practices for the future.
For OTs who have additional concerns about practicing telehealth or who are left in the dark about their own state’s regulations, the AOTA has temporarily granted access to some “member only” articles about telehealth practice.
Initial Evaluation in Virtual Form: Benefits and Barriers
Virtual evaluations come with a few logistical benefits including schedule management, accurate timing sessions for billing purposes, and the more rapid ability to collect and organize results in one location. In fact, there are several popular pediatric evaluation tools available in an online format.
However, there is a downside to a purely virtual evaluation especially for brand new clients and patients with physical limitations. The OTs and the patients miss out on the hands-on data collection including ROM testing, MMT testing, sensory testing, and so on.
Changes to Training, Certification, Licensure, Hiring
Many healthcare professionals have hit training and certification-related barriers. Recent graduates also are facing challenges. Testing dates have been postponed/rescheduled and fieldwork hours have been left incomplete, which has forced a huge body of future clinicians into an unemployed limbo. Even if students have met graduation requirements, have gotten certified, and have received their licenses, some companies aren’t hiring at the rates they used to.
Although NBCOT resumed normal certification testing at the beginning of May, some prospective OTs are still experiencing delays. On the plus side, the AOTA has been tracking OT Licensing Boards and Legislative updates due to the COVID-19 pandemic.
Such updates include extended licensing periods without having to meet continuing education requirements, obtaining temporary licenses to volunteer across state lines, and obtaining temporary practice licenses for a given period.
Estimated Amount of Visits Forced to Shift to Strictly Virtual
I live in rural America and typically work with patients in short-term and long-term skilled nursing. For me, there’s been no significant shift in my schedule or virtual transitions with patients. Other OTs across the nation, especially working in outpatient and home health settings in larger cities have a different experience.
Facilities, schools, and other rehabilitation settings have been forced to shift some or all in-person visits to virtual visits. The number of virtual visits versus in-person visits has been temporarily determined by insurance policies, most of which have been providing temporary waivers, coding guidelines, and interactive (audio plus video) rules.
The ratio between in-person and virtual visits varies by state and setting. For example, some school districts may require only one in-person visit for EIPs while mandating all other OT visits be virtual.
PPE Increase and Investment in OT Practice
Depending on the practice setting, OTs have to either reinforce or complement their clinical time with appropriate personal protective equipment (PPE) measures. Such standards are decided for them by upper management based on CDC recommendations and OSHA regulations.
PPE goes beyond the face mask and bottle of hand sanitizer. Depending on an OT’s exposure risk and their patient population, there could be an increase in gloves, facial shields, goggles, air lines, and disposable gowns. Not only are OTs investing in the equipment itself, but in the time it takes to maintain, stock, dispose of, sanitize, and educate caregivers and patients on safe use.
What’s Next?
The year 2020 has become an unpredictable hurricane of last-minute changes. We are all working hard to stay on top of a shifting ecosystem. On the bright side, we can take comfort in knowing that we are all experiencing the same bumpy ride. Moving forward, the OT community can help decide which pandemic-esque changes we should keep that will have lasting positive impacts on our profession.


