Medication calculation goes far beyond the NCLEX in terms of importance to your nursing career. You’ve already passed at least one in nursing school, likely before you were able to touch a patient in clinicals. Once you’ve started orientation for your new job, you will almost certainly have to pass another, more substantial med calc test. Beyond simply being tested on medication calculation, it is an invaluable skill that will save your patient’s lives (as well as your license!). With the advent of electronic medication administration records and computerized medication dispensaries (like a Pyxis), it’s easy to get complacent and defer your own calculation in favor of what the eMAR tells you to administer. However, it’s good practice to always double check the math. Perhaps the Pyxis experienced a glitch. Maybe the provider ordered the wrong dose. What if the pharmacists sent the incorrect concentration? You are the last line of defense protecting your patients from preventable harm. Do not shirk this responsibility!
We’ll use examples to talk how about the important equations you need to remember for the NCLEX and your nursing practice. The central tenet of medication calculation is to simply align your equation so that the necessary units “cancel out” and you’re left with the desired unit. The types of medication have been left out to decrease distractors.

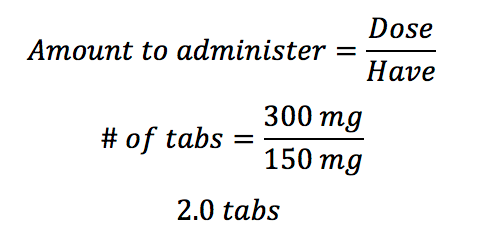
The patient is ordered to receive 300mg of a medication. The medication comes in 150mg tablets. How many tabs will you administer to the patient? Write your answer to the nearest tenth decimal place.
The simplest equation in medication calculation is this:
The patient is ordered to receive 0.45 mg of an intravenous medication. The vial states that the concentration is 3mg/mL. How many mL will you administer to the patient?
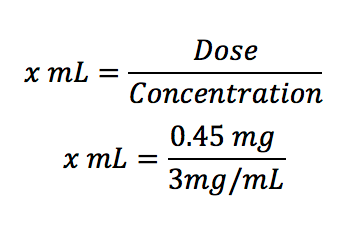
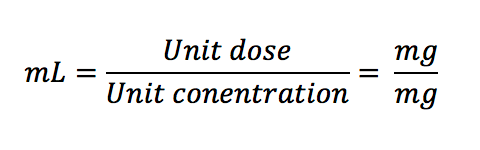
This is the same as the equation below, but all the units are aligned and easy to see:
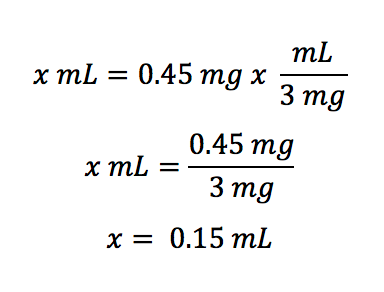
A shortcut for this equation is to simply think in your head (or on paper):
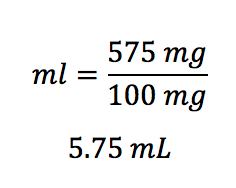
The patient is ordered to receive 575 mg of an infusion that must first be diluted with 10 mL of sterile water. Once mixed, the volume in the bottle is 11 mL. There are 1100 mg in the vial. How many mL does the patient require?
A lot of words in this question, right? Break it down like this:
- What is the ordered dose? It’s 575 mg
- What is the available concentration? It’s 1100 mg/11 mL, or 100 mg/mL
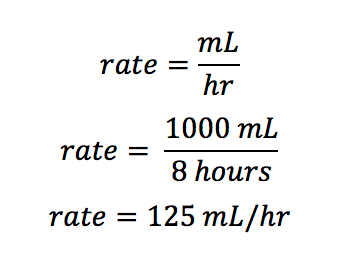
The patient has been prescribed 1000 mL lactated ringers over 8 hours. At what rate should the nurse program the IV pump?
This one couldn’t be easier. The final answer will have the unit of mL/hr, right?
As a general rule, IV infusions are administered using an IV pump that runs in mL/hr. However, you will be asked questions regarding drip rates and drip factors. Use this equation:
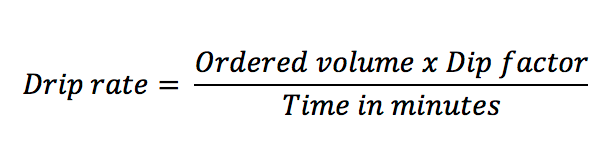
You will generally be given the IV tubing set’s drip factor (frequently 10 gtt/mL, 15 gtt/mL, or 60 gtt/mL), the dose, and how quickly the medication should be infused. From there, it’s as simple as plugging in numbers!
The patient is prescribed 600 mg of an antibiotic over 2 hours. The drug comes in a concentration of 600 mg in 50 mL. The IV tubing’s drip factor is 15 gtt/mL. What is the drip rate for this infusion?
There are some distractors here. The patient will receive 600 mg of a 600 mg bag of IV fluid. But, there is no space for the milligrams in the equation, so we will leave that out. The equation requires time be in minutes, so we must convert 2 hours to minutes prior to starting the equation.
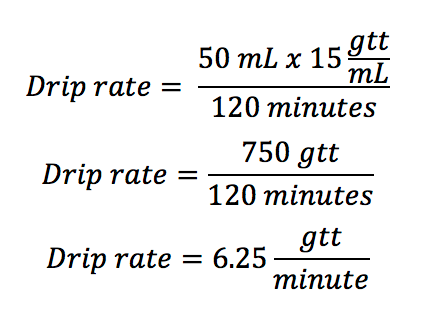
You’ll administer 6.25 drips/minute. Wait. What? How are you going to administer a quarter of a drip? You’re not! Always round your drip rate up to the nearest whole number. Therefore, the drip rate is 7 gtt/min.
Due to the differences of drug absorption and metabolism in children, pediatric dosing is based on weight. For questions involving children, the dose will be written in unit/kg. One of the NCLEX test writers’ favorite distractions is to give you the child’s weight in pounds rather than kilograms. This is a simple conversion:
Here’s an example:
The 56-lb. child is prescribed 50 mg/kg of a medication available in 100 mg/mL concentration. How many mL will the nurse administer to the patient?
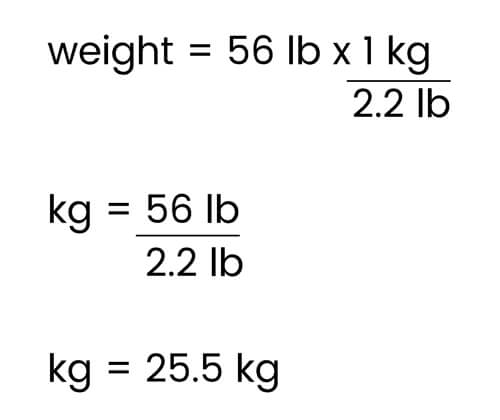
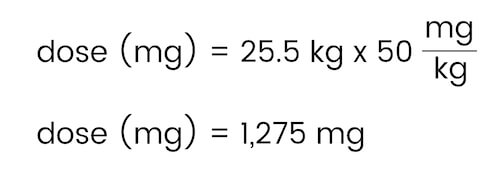
First, determine the patient’s weight in kilograms:
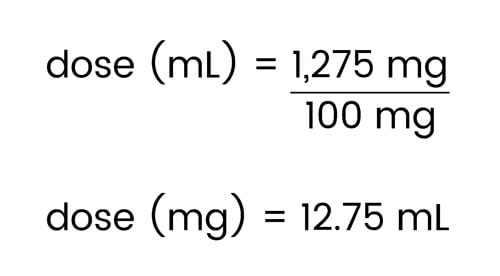
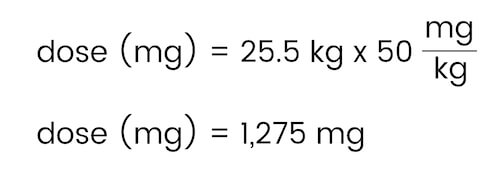
Now, determine the patient’s dose:
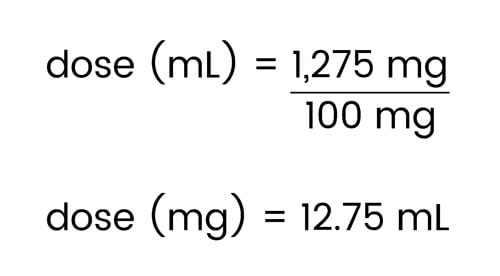
Finally, use the medication concentration to calculate the amount in milliliters to be administered.
As with any NCLEX concept, repetition is key. Keep answering medication calculation questions until it becomes second nature to you. Figure out which tricks work for you and stick with them. Don’t get bogged down with the minutiae that inevitably accompanies NCLEX medication calculation questions. Remember, medication calculation questions don’t only exist on the NCLEX. Medication calculation is a skill required to be a safe and competent nurse, so don’t shrug it off. Your future patient’s lives depend on it!

