If you’re unsure what to study for the AACN PCCN exam, keep reading as we will give you some pointers. The PCCN exam is a 2.5-hour test with 125 (100 scored) multiple-choice items. The PCCN exam focuses solely on adult patient populations.
American Association of Critical-Care Nurses (AACN) provides candidates with a detailed PCCN Exam Handbook which is also outlined below.
1. Clinical Judgment (80%)
A. Cardiovascular (33%)
B. Pulmonary (14%)
C. Endocrine/Hematology/Gastrointestinal/Renal (18%)
D. Neurology/Multisystem/Behavioral (15%)
2. Professional Caring and Ethical Practice (20%)
A. Advocacy
B. Caring Practices
C. Collaboration
D. Systems Thinking
E. Response to Diversity
F. Clinical Inquiry
G. Facilitation of Learning
1. Cardiac Blood Flow
While it’s a little silly, we LOVE this video demonstrating blood flow through the heart. Just like a number one hit on the radio, if you listen to it a few times you’ll likely remember it. Just don’t get caught singing during the PCCN exam!
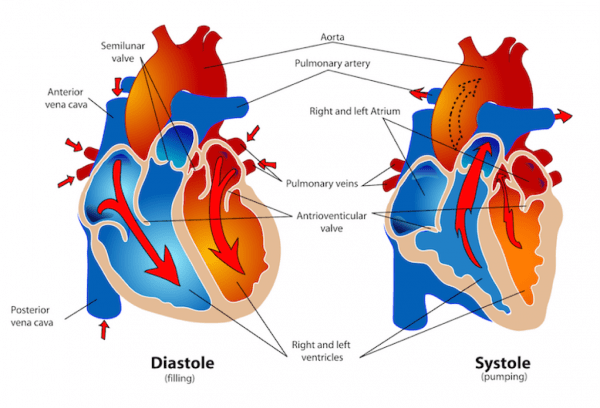
2. Events during Diastole / Systole
A. Diastolic Filling Phase
• The cardiac muscle gets its perfusion during diastole. Perfusion is determined by coronary perfusion pressure.
• Coronary Perfusion Pressure = Diastolic BP – PCWP
• Normal: 60-80 mmHg
B. Systolic Ejection Phase
During systole, the cardiac muscle has to overcome the pressures ahead of each chamber. The right ventricle meets low to no pressure in the lungs. The left ventricle must overcome the diastolic pressure in the aorta.
3. Hemodynamics
• Cardiac Output = HR x Stroke Volume (SV)
• Normal Cardiac Output: 4-8 liters/minute
• As cardiac output decreases, heart rate increases. Heart rate is controlled by stimulation of both the sympathetic and parasympathetic nervous system.
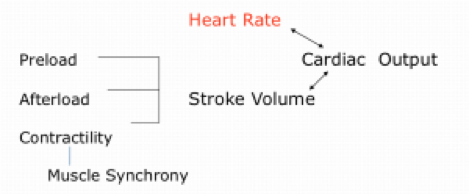
4. Stroke Volume (SV)
• Stroke Volume: The amount of volume ejected by the ventricle with each systolic contraction OR amount of blood ejected by the heart with each beat.
• Normal: 60-130 mL
• SV = (CO/HR) x 1000
5. Preload & Afterload
A. Preload
• The force on the ventricle during relaxation (diastole)
• Primary determinant is the volume of blood filling the ventricle
• Right Ventricle = RVEDP (Right heart preload)
• Right Atrial Pressure (RAP); CVP
• Normal values: 2-6 mmHg
• Left Ventricle = LVEDP (Left heart preload)
• PCWP, PAWP, or PAOP
• Pulmonary Artery Diastolic (PAD)
• Left Atrial Pressure (LAP)
• Normal values: 8-12 mmHg
B. Afterload
• Afterload: The ventricular force or pressure required to overcome impedance to ejection
• As impedance increases, ejection velocity, and SB decrease, while ventricular workload and O2 consumption increase.
• Systemic Vascular Resistance (SVR): Left
• Normal SVR: 900-1400 dynes/sec/cm-5
• Pulmonary Vascular Resistance (PVR): Right
• Normal PVR: 50-250 dynes/sec/cm-5
6. Anticoagulants
• Patients with mechanical valves will require lifetime anticoagulation
• After a mitral valve replacement, patients are likely to have anticoagulants as a plan of care.
7. Genetic Cardiac Disease
A. Long QT Syndrome
B. Brugada Syndrome
8. Wolff-Parkinson-White Syndrome
• Wolff-Parkinson-White (WPW) Syndrome is a condition in which episodes of fast heart rate (tachycardia) occur due to an abnormal extra electrical pathway in the heart.
• Extra electrical pathway between the atria and the ventricles (accessory pathway)
• Symptoms (not always present) may include: Palpitations, dizziness, lightheadedness, and fainting